Matters of the Heart - Cardiac Arrest
Cardiac Arrest
So, the last thing we discussed was Sinus Rhythms, but now we are going to its antithesis, and every nurse's nightmare, Cardiac Arrest!!
I’ve got your attention now, huh? Lol! Cardiac Arrest is scary, I’m sure we all can agree with this. However, if we can approach cardiac arrest with knowledge, we can have less fear, or even prevent it all together. Let’s start with the basics.
What is Cardiac Arrest?
Cardiac arrest is a sudden stop in the function of the heart. This could mean the heart has completely stopped beating, or that its activity is not significant enough to support complete contractions or sustain life.
Of course, cardiac arrest is an emergency. I’ll go as far to say that is one of the main “big” emergency medical situations.
What causes Cardiac Arrest?
Oh, if only I had the time to spell out every single thing that could cause cardiac arrest. The truth is, a lot of things can lead to cardiac arrest. However, there are a few basics that we know can lead to cardiac arrest, can you guess where I’m going with this?
The ABCs! An obstruction or issue that compromises the body’s ability to carry out the ABCs will lead to cardiac arrest.
Airway:
Pulmonary Edema - An excess of fluid in the lungs, which can compromise oxygenation and eventually lead to cardiac arrest, if left untreated.
Airway obstruction by an object or disease process.
Collapsed lung/pneumo or hemothorax - the lungs collapsing under the pressure from excess air or blood around one lung can lead to an eventual cardiac arrest if the problem is not corrected.
Breathing:
Apnea - lack of breathing
Untreated and sustained tachypnea - Rapid breathing, in excess of 25-30 breaths a minute.
Untreated and sustained Bradypnea - Slow breathing rate, less than 10-12 breaths a minute.
Circulation:
Cardiac Tamponade - The heart becoming surround in excess blood or fluid can restrict movement of cardiac muscle and lead to cardiac arrest.
Ventricular Dysrhythmias - Abnormal heart rhythms, when left untreated, can lead to cardiac arrest. In my practice, the most common arrest rhythm has been ventricular fibrillation (V-fib).
Coronary Artery Disease - Poor perfusion of cardiovascular muscle can lead to a stalling of the heart.
Myocardial Infarction - The acute and significant damage of cardiac muscle, as the result of an acute blockage in the coronary arteries, can halt the hearts pumping ability.
Congenital Heart Disease - Heart conditions that occur from birth, such as Tetralogy of Fallot, can cause circulatory issues, due to malformed muscle and valve structures in the heart.
Heart Failure - A lack of strength in cardiac muscle to produce substantial cardiac output, will lead to cardiac arrest, if untreated.
Cardiomyopathy - Thickening or dilation of the ventricular muscles can restrict and limit the heart and its ability to pump blood effectively.
Heart Valve Disease - Weak heart valves that leak can cause the cardiac muscle to become weakened and stretched, leading to progressive ineffective pumping.
Other Causes?
Extreme Hypothermia - reaching an internal temperature that is too low.
Drug interactions and overdoses from cardiovascular drugs, such as digoxin and procainamide.
Electric Shock - An external electric shock can cause the heart to stop or go into a lethal arrhythmia.
Electrolyte imbalances - An Imbalance of electrolytes, such as calcium, potassium, and magnesium, can cause cardiac dysrhythmias and lead to cardiac arrest.
So, What does cardiac arrest look like?
Well, interestingly enough cardiac arrest does not always present in the same way on an ECG. Not every cardiac arrest will be the classic “flatline” asystole. Surprise! Did you know that? I bet you did! If you didn’t know this, it’s OK we’ll cover some of the different ways cardiac arrest can present.
Example 1: Asystole: The rhythm that’s essentially the absence of a rhythm, or electrical activity, in the heart. This is the infamous “flatline” wave we see the most on TV medical dramas (even though it is presented in the most inaccurate ways).
(Source)
If you learn nothing from our series, please remember, we do not shock asystole.
We do CPR and give meds, but we do not shock it, like they do so frequently on TV.
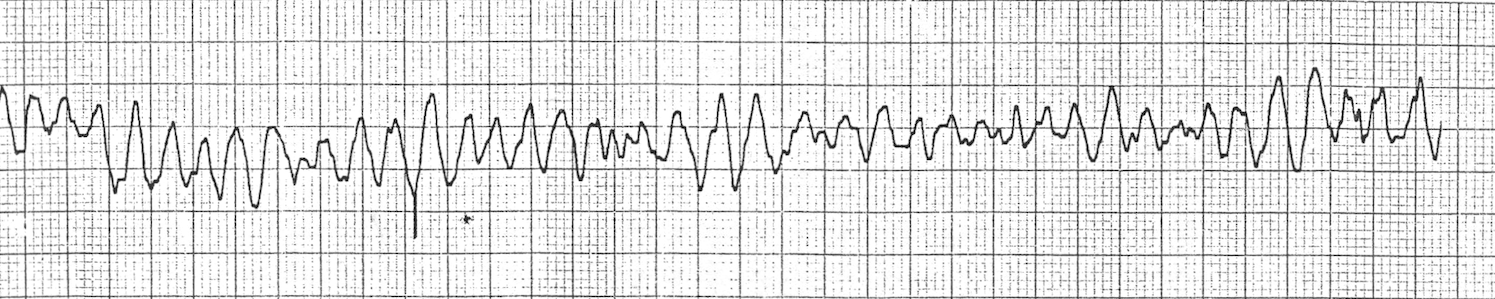
Example 2: Ventricular Fibrillation
This is a Rhythm that we will discuss more, in a later post. Ventricular Fibrillation, also referred to as V-Fib, is the chaotic discharge of electrical impulses in the heart, to the power chambers of the heart, the ventricles. During v-fib, the ventricles are simply quivering and not moving blood at all, thus it is considered an arrest rhythm. I always remember this rhythm by thinking of how my 2nd-grade teacher used to call my cursive, handwriting chicken scratch (it was pretty bad) and this is what it would look like. Lol!!!
(Source)
Example 2.5: Little tidbit, V-fib can present as coarse, which is pictured above, or fine, where the ECG almost looks like asystole, yet there are small and noticeable waves that look like a lot of lower case n’s strung together.
Here is an example of fine v-fib.
(Source)
Example 3: Pulseless Ventricular Tachycardia (V-tach or VT) rhythms.
V-tach indicates that rapid electrical impulses are firing in the ventricles, causing rapid beating of the lower chambers of the heart, the ventricles. V-tach, when present with a pulse, can be episodic, lasting for a few seconds, or sustained. It is classified by having 3 or more premature ventricular contractions (PVCs) in a row, with a rate greater than 100bpm. If someone is experiencing frequent short runs or sustained V-tach, and they still have a pulse, you have a little time, but not much. You will need to act quickly to prevent the patient from decompensating. V-tach tires the heart quickly and, if left untreated, will quickly result in pulseless v-tach or another fatal rhythm.
Pulseless v-tach is an arrest rhythm that can manifest in 3 different ways. I know that sounds like a lot, but they all look completely different, thus they are not hard to differentiate, visually.
Example 3.1: Monomorphic V-tach - The QRS complexes are usually the only visible waves. The complexes will be wide and will be approximately the same size and uniform in their presentation.
Note: I have always thought that V-tach looks like someone copied and pasted a lot of drawings of big, tall, and lopsided hills together, like this…
(Source)
Note that the rhythm and pattern are fairly regular in nature.
Example 3.2: Polymorphic V-tach - This is a weird looking rhythm, where the QRS complexes remain the primarily visible waves, but they are different sizes and widths. The reasons for this is explained in another post on V-tach. Here’s a picture of polymorphic V-tach.
(Source)
Note that the rhythm appears to be becoming less regular.
Example 3.3: Torsades de Pointes - Besides having the fanciest name, this rhythm is easiest to remember, because of its awkward manifestation on the ECG strip.
Note: It has always put me in mind of the way the waves look on a recording device, as someone’s pitch and volume goes up and down. [I realize my method of memorizing stuff may be wacky. But hey, it helps it stick in my brain! Lol!]
(Source)
This rhythm is characterized by an irregular rhythm, with QRS complexes of varying size, amplitude, and width. It’s known for its undulating (up and down wave) appearance.
Example 4: Pulseless Electrical Activity (PEA): PEA is when there are electrical impulses in the heart, but the muscle is not responding to these impulses. This little deceptive devil can mimic many rhythms, yet there is no mechanical or pumping activity in the heart. As PEA continues, the rhythm typically evolves into a more erratic and irregular rhythm. The QRS complexes will become progressively smaller and wider, and PEA will eventually turn into asystole.
Now that all of that rhythm talk is done, let’s get down to what we can do about cardiac arrest.
What are the signs and symptoms of cardiac arrest?
Thankfully, no matter how complex the ECG rhythms for cardiac arrest may seem, the clinical and physical manifestations are pretty obvious.
Just before cardiac arrest, a patient can experience acute anxiety and feelings of impending doom, and so can nurses.
Signs and symptoms:
No pulse or heartbeat. The primary way to verify this is by palpating pulse at the carotid artery or femoral artery in the groin. Some places may also use Dopplers to assess the presence of a pulse. Finally, a lesser common method in emergent situations is to auscultate the chest vanity for heart sounds.
An unresponsive patient.
A patient that is not breathing on their own.
No cardiac output, unable to obtain VS, and no organ perfusion.
Nursing interventions/Considerations for Cardiac Arrest:
Nursing interventions, in regards to Cardiac Arrest, will include a nursing physical assessment, repetitive and frequent monitoring of vital signs (particularly before an arrest), and activation of your facility emergency response system, and begin to use and follow the ACLS Algorithms.
Ensure the patient’s safety
Activate (or send someone else to activate) emergency response system at your place of work.
Avoid leaving the patient alone.
Have someone bring the crash cart and intubation box (if they are kept separate).
Start CPR immediately after assessing that your patient is unresponsive and there is no heartbeat or respirations.
Establishing a rotation for CPR. Set-up Ambu bag and attach it to oxygen. Place Defibrillator pads on patient’s chest.
If someone is free, it is nice to ask them to remove unnecessary furniture, equipment, and people out of the room or at least away from the patient area where the arrest is happening.
Once the emergency response team arrives, the patient’s primary nurse should be free from any other task and be available to update the response team on the events that lead to the arrest, the patient’s reason for admission, relevant history and significant events reported at shift change.
Having a report or brain sheet with all of this information can help with staying focused, despite the adrenaline rush. Keep your report sheet on you, at all times.
Some EHR systems may have a section with information like this available.
Treatment: Meds/Tests/Imaging
Treatment of Cardiac Arrest focuses on 2 things, the first is the restarting of the heart and the second identifying and treating the source of the dysthymia or other issues that caused the arrest.
CPR - CPR is the principal treatment for cardiac arrest.
AED/Defibrillation - Shocking the heart to induce a return to a rhythm more compatible with life is an option with some cases of cardiac arrest.
It should be noted, that PEA and Asystole are not shockable rhythms. Treatments for these occurrences focus around quality CPR and medications
Pharmacological Options: Most of these are ACLS Drugs
Atropine
Magnesium
HCO3 - Bi-Carb
Extended care after Cardiac Arrest
Of course, patients experiencing cardiac arrest that achieve a return of spontaneous circulation (ROSC), will need to be admitted into an intensive care unit (ICU).
Management post-arrest will focus on continuing to isolate the cause of the arrest or dysthymia. Supportive treatments for maintained blood pressure and cardiac output will be ordered. Vasopressors/vasoactive infusions and drips (gtts) will be ordered.
The patient will very likely be intubated and on a sedative.
Sources
ECG Interpretation Made Incredibly Easy! Pocket Guide
Emergency & Critical Care Pocket Guide ACLS Version 8th Edition
Critical Care Nursing Demystified
Practical Clinical Skills Website
Disclaimer: This material should be used to supplement your understanding of the cardiovascular system. Any use of the information given in this post series is at your own risk and should be verified prior to making it a part of your nursing practice. There may be affiliate links associated with some products but we promise that we will never recommend anything that we don’t use ourselves.