Matters of the Heart - Calcium Channel Blockers
As the name suggests, Calcium Channel Blockers (CCBs) block calcium.
Cells move calcium across their cell walls via calcium channels, creating electrical activity and contracting the cell. CCBs stop this action from happening thus sending less impulses (decreasing the heart rate) and relaxing the cardiac cells (vasodilating).
So you give CCBs for tachycardia and/or hypertension. Makes sense right?
Wouldn’t pharmacology be so easy if that were the only thing we needed to know?
But you and I both know it is NOT all we need to know, so say goodbye to that dream.
The good news is that I have covered what you DO need to know. So let’s become versed in Calcium Channel Blockers, shall we?
Calcium Channel Blocker List
Here is a list of the CCBs you should know:
Notice after the first two listed, all the other names end in -dipine. So the list you really need to remember is:
Verapamil
Diltiazem
-dipine
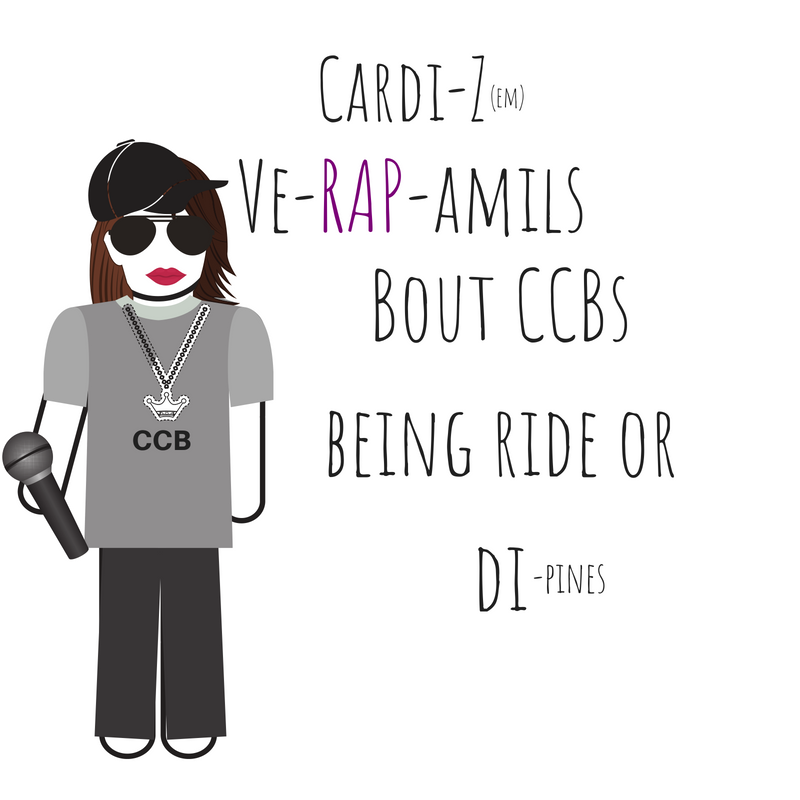
In my practice, I have only ever called Verapamil by its name, Verapamil. Diltiazem, however, can be called a few things. I have called it “Dilt” and by its brand name “Cardizem.”
I am going to just leave my personal thought process I have for memorizing the CCB list below in a picture:
Anyway…
Classification “types”
There are three types of Calcium Channel Blockers (CCBs). So the same way we are remembering the names with only knowing 3 basic names, is how they are classified as well. Easy peasy lemon squeezy!
They are separated into by their chemical makeup. I don’t think it is important to remember the class name or that it is a chemical makeup of the drug but I think it is important to know that they are different and which one is used is based on chemical makeup because there are different indications and side-effects. Below I listed them for classification purposes:
Calcium Channel Blocker Classification
Phenylalkylamine- Verapamil
Used primarily to treat angina by reducing the heart's oxygen demand and reversing coronary vasospasms.
Works by decreasing the force of contraction in the heart (not by vasodilating)
Contraindicated with beta-blockers
Benzothiazepine- Diltiazem
The mechanism of action is a mix between Phenylalkylamines and Dihydropyridines.
Works by vasodilating and decreasing the force of the heart.
Dihydropyridines-(end in -dipine)
This class of CCBs is most selective for smooth muscle (meaning going to decrease systemic vascular resistance) and used primarily for hypertension.
Sometimes this can cause hypotension and this leads to the heart speeding up to fulfill the body’s oxygen demand. This is called reflex tachycardia.
There are three generations of Dihydropyridines:
1st generation
Nifedipine
2nd generation
Nicardipine
Felodipine
Isradipine
3rd generation
Amlodipine
How do Calcium Channel Blockers work?
When a CCB is distributed into the bloodstream and flows to the heart, it attaches to the calcium channels. This stops/slows the calcium from flowing through cell walls into the cells. Calcium channels are found in abundance at the SA and AV nodes as well as in cardiac myocytes, and smooth muscle cells.
SA and AV nodes are the pacemakers of the heart, so if your patient has tachycardia due to a problem above the ventricles (supraventricular) then a CCB may help. When calcium is slowed from crossing into the SA or AV node cells, electrical activity will slow down, decreasing the rate of impulses being sent out to contract the heart. This will inherently increase the refractory period of the AV node (increasing the PR interval) and decreasing ventricular response.
Smooth muscle cells found around blood vessels control vasodilation and constriction. Blocking calcium intake into the cell relaxes the smooth muscle, opening up the blood vessel and decreasing blood pressure.
Oh and guess what else smooth muscle controls?
Your poop.
Smooth muscle is also located in your GI tract and slows down your gut motility. So these patients can have constipation.
Note: Skeletal muscle uses sodium influx for contraction, not calcium, and is not affected by CCBs.
Calcium Channel Blocker Uses and Indications
Now that we know what Calcium Channel Blockers do, it should be pretty easy to answer the question: Why would I administer a calcium channel blocker to my patient?
Answer: If they have high blood pressure or a fast heart rate, you would administer a CCB.
For example in these conditions:
Hypertension
Because it decreases BP
Angina
Vasodilation will help get blood through any partially occluded vessels so if the chest pain is from decreased blood flow to a part of the heart, CCBs will open up the vessel more and allow more blood to get through
Supraventricular tachycardias
Because it decreases heart rates and works at the SA and AV nodes so if the rhythm is above the ventricles it is likely occurring from the SA or AV nodes and this will decrease the stimulus, thus decreasing the heart rate
Administration of a Calcium Channel Blocker
A Calcium Channel Blocker can be administered orally or intravenously. You will not be administering oral CCBs in an emergency but you might administer IV CCBs in a non-emergency.
Giving IV Calcium Channel Blockers:
Verapamil
5-10 mg IV push over 2 minutes
Diltiazem
Stand-alone bolus:
0.25mg/kg over 2 minutes
Bolus followed by infusion:
Usually 10-20 mg over 2 minutes
Infusion:
5-10 mg Infusion with bolus (see dose above)
Increase by 5-10 mg every 15 minutes as needed until the desired heart rate and BP are reached.
When giving a Calcium Channel Blocker you should monitor heart rate, blood pressure, and digoxin levels. This is because of the potential of the BP bottoming out, heart rate slowing down too much and of course, this medication makes digoxin levels higher. So keep your eye on your patients dig levels if they take digoxin.
Calcium Channel Blocker Side Effects
Increases Digoxin levels
Digoxin also binds to the same calcium channels that CCBs do, except that CCBs have a stronger affinity, kicking digoxin off the binding site and causing potentially lethal serum digoxin levels.
Constipation
Remember smooth muscle involvement!
Hypotension
Smooth muscles relaxing causing dilation.
Bradycardia
Slowing conduction through the SA and AV nodes
AV node block
When the blocked channels completely stop the AV node from communicating to the ventricles. The Purkinje fibers will take over as the pacemaker at this time so the heart rate will be slowwwww (20-40 bpm).
Congestive Heart Failure
Patients with CHF need to have an increase in the force of contraction. So decreasing the force of action plus vasodilation will compound the CHF.
Edema
Vasodilation will increase edema because it makes the capillaries leaky, making the surrounding tissues fill up with fluid.
Heartburn
The smooth muscles being relaxed can cause the esophagus to relax too, meaning GERD.
A headache
From vasodilation, increase in blood flow can cause headaches (like with nitroglycerin!)
Flushing
From vasodilation, increase in blood flow to the surface of the skin.
Calcium Channel Blocker Overdose
Any calcium channel blocker overdose is serious, however, the most concerning (and most lethal) to overdose on are verapamil and diltiazem because they inhibit metabolism leading to a long half-life.
CCB overdose is no joke because the medications usually have a sustained release action as well. So if symptoms start to occur, they will continue to get worse because there is more of the medication to be released.
Symptoms
Hypotension
Cardiac Dysrhythmia
Bradycardia
Heart Blocks
Central Nervous System Effects
Confusion
Altered Mental Status (AMS)
Syncope
Seizures
Coma
Nausea and Vomiting
Hyperglycemia
Insulin release is dependant on calcium influx into beta-islet cells so when the calcium channels are blocked, insulin is not released.
Antidote
Calcium Chloride (note: NOT calcium gluconate)
1gm over 5 minutes repeated every 15-20 minutes as needed for 2-4 doses
Goal: To keep serum calcium levels <11 mg/dL
Monitor: For the pulse to normalize
Stop giving Calcium Chloride if calcium serum levels go above 11 mg/dL
Glucagon
Used for medications that cause a decrease in intracellular calcium (soooo CCBs falls in this list!) when the heart rate is too bradycardic
Increases cardiac contractility
Increases cardiac heart rate
Other Treatments
Fluid boluses of normal saline or lactated ringers
Cardiac pacing as needed
Atropine for SA node bradycardia (Note: doesn’t help for AV node bradycardia)
Vasopressors (Dopamine or Norepinephrine)
Insulin as required to reduce blood sugars and increase myocardial carbohydrate metabolism
Start with a bolus of short-acting insulin at 1 Unit/kg
Then have an insulin drip start at 0.5 Units/kg/hr and titrate up every 30 minutes up to 5 Units/kg/hr.
Can be up to 850 units/hr of insulin!!! Yeah, you read that right. Insulin therapy is aggressive
Closely monitor patient glucose levels and add IV glucose such as D5W as needed to help the patient have normal serum glucose levels
Consider activated charcoal if very early in the process and the patient is asymptomatic.
If it is an extended release (ER) than it can be up to 4 hours after ingestion of the CCB
If it is not an ER medication than you can administer activated charcoal up to one hour after ingestion, safely.
Calcium Channel Blocker Contraindications and Considerations
Calcium Channel Blockers (CCBs) should be given with caution in patients with kidney disease because the kidneys excrete out the medication. So if the kidneys are not working, the CCBs will stay in the blood and body.
Make sure you have obtained an EKG before administering a CCB to someone who has never had this medication. If you are administering the medication IV, get an EKG regardless if they take the medication at home or have had the medication before. You are looking for AV block (second or third degree heart block) and sick sinus syndrome on the 12 lead ECG/EKG. If the patient has AV block or sick sinus syndrome, do not give this medication.
Take vital signs prior to administering this medication. If the patients blood pressure or heart rate are low, hold the medication.
Withdrawing CCBs needs to be done in a slow and controlled manner because a patient can revert to dangerous arrhythmias if discontinued abruptly.
Also, do not give with grapefruit juice. I threw this in there because as a nurse, you may need to teach the patient to not do this. Side note: if you work in a hospital that serves grapefruit juice, I want to hear about the other fancy things you have so please leave a comment and let me know.
Long-term considerations for Calcium Channel Blockers
Patients who are on calcium channel blockers will likely need BP and heart rate monitoring by the primary care team. The patient may also need to be prophylactically treated for constipation (remember CCBs slow down gut motility because they attach to the smooth muscles in the intestines).
Disclaimer: This material should be used to supplement your understanding of the cardiovascular system. Any use of the information given in this post series is at your own risk and should be verified prior to making it a part of your nursing practice. There may be affiliate links associated with some products but we promise that we will never recommend anything that we don’t use ourselves.
Sources:
Written by: Susan DuPont of BossRN.com who is a full-time nurse in a level I trauma Emergency Room. In her spare time, she loves the outdoors, fishing, and hunting.